
Recently, many patients with varicose veins have sought medical attention. Regardless of whether they undergo surgery, they need to prevent the condition in their daily lives. Therefore, I would like to share some knowledge about varicose veins in the lower limbs and how to properly wear medical compression socks.
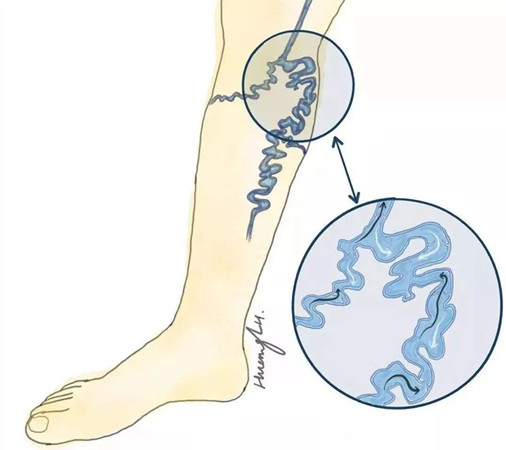
Varicose veins in the lower limbs refer to the dilation, elongation, and twisting of the superficial veins in the lower limbs, which can lead to chronic ulcers in the later stages. This condition is common among people who stand or bear weight for long periods, such as teachers, doctors, nurses, waitstaff, and chefs. Early-stage varicose veins, apart from the visible superficial vein dilation, or “bulging blue veins,” generally have no symptoms. However, as the condition progresses (usually over several years to a decade), its harmful effects gradually become apparent. Common severe symptoms include edema, skin pigmentation/dermatitis, bleeding, chronic ulcers, and thrombophlebitis.
The formation of varicose veins in the lower extremities is multifaceted, mainly due to the following reasons:
Genetic factors, congenital developmental defects, weak vein walls, and venous valve defects;
Postnatal lifestyle habits affect long-standing, long-sitting, local trauma or patients like to cross their legs, causing local veins to be compressed and injured;
There is a history of lower limbs being soaked in cold water for a long time, or combined with long-term asthma, constipation or heavy physical labor, causing long-term abdominal pressure to increase;
Women have been pregnant many times, and the abdominal pressure increases during pregnancy, causing venous valve insufficiency, leading to blood reflux, and then the pressure of the lower extremity veins increases. Capillary proliferation in the ankle, increased vascular permeability, red or blue skin on the legs like spider webs, and twisted blood vessels like earthworms. Blood exudation leads to pigment deposition and lipid sclerosis.
Varicose veins in the lower extremities Complications of varicose veins in the lower extremitiesIf varicose veins in the lower extremities are not treated in time, thrombotic superficial phlebitis will occur. After 20-40 years of chronic varicose veins, nutritional changes in the skin of the lower extremities, especially the ankles, such as skin atrophy, leg hair loss, desquamation, skin and subcutaneous tissue lipid sclerosis, eczema, varicose vein rupture bleeding and ulcers, etc., patients should be treated as soon as possible.
C1: Capillary dilation or spider-like venous dilation;
C2: Varicose veins in the lower extremities;
C3: Varicose veins in the lower extremities and swelling of the lower extremities;
C4: Varicose veins in the lower extremities and skin damage changes;
C5: Varicose veins in the lower extremities and ulcer healing period;
C6: Varicose veins in the lower extremities and ulcer active period. Prevention of varicose veins in the lower extremities The prevention methods of varicose veins in the lower extremities are not so complicated, they are very life-oriented, and the key is to persist.
The methods for preventing varicose veins in the lower extremities are not overly complicated and are quite practical in everyday life. The key is consistency. Avoid sitting or standing for extended periods, and elevate the affected limb during rest. The principle behind this is to reduce the pressure in the veins of the lower extremities. Walking can effectively prevent varicose veins.
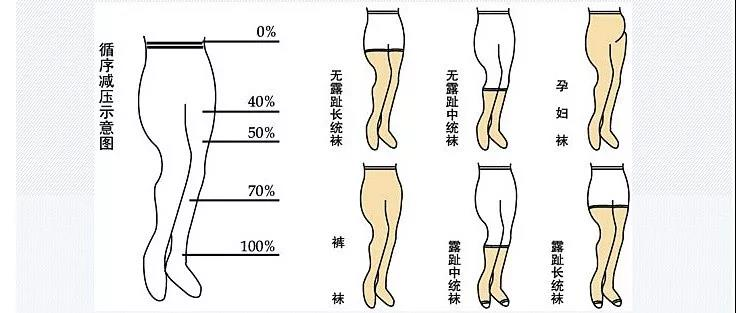
Wearing medical compression stockings consistently can have both preventive and therapeutic effects. They can effectively promote blood circulation in the lower extremities, reduce venous dysfunction in the affected area, eliminate blood stasis in the lower extremities, and alleviate discomfort such as fatigue and swelling after standing for a long time. This can delay the progression of varicose veins and support the recovery period after vein stripping surgery in the lower extremities.
Medical compression stockings work by using a professional pressure gradient design. They establish the highest support pressure at the ankle and gradually decrease up the leg. The pressure reduces to 70%-90% of the maximum at the calf and to 25%-45% of the maximum at the thigh. This decreasing change allows the venous blood in the lower extremities to flow back, effectively relieving or improving the pressure on the veins and venous valves in the lower extremities. By contracting the calf muscles to increase pressure on the blood vessel cavity, it promotes the return of venous blood to the heart, prevents venous congestion in the lower extremities, ensures good blood circulation in the veins of the lower extremities, and promotes the disappearance of symptoms such as swelling and pain in the affected limbs.
Those who stand for long periods, such as teachers, nurses, sales associates, servers, traffic police, etc.
Those who sit for long periods, such as office workers, including white-collar workers and civil servants.
Pregnant women and those who take birth control pills for a long time.
Frequent travelers, especially those who often take long flights or bus rides.
Overweight individuals.
Those who already have lower extremity venous diseases.
Those at high risk for deep vein thrombosis in the lower extremities.
Patients with peripheral arterial disease.
Those with poor skin conditions on the lower limbs, such as fragile “paper-like” skin, local inflammation, gangrene, recent skin grafts, local infections, etc.
Those allergic to compression stockings.
Those with heart failure.
Compression stockings are divided into three pressure levels: low, medium, and high. Low pressure (preventive, 18mmHg) is mainly used to prevent feelings of heaviness and fatigue in the legs, varicose veins, thrombosis, and embolism, as well as to prevent economy class syndrome. It can also be used to treat mild edema and mild varicose veins during pregnancy. Medium pressure (therapeutic, 20-30mmHg) is suitable for patients with obvious varicose veins in the lower extremities, superficial phlebitis, or those with deep vein valve insufficiency. It is also suitable for patients who have healed from lower extremity venous ulcers after treatment. High pressure (therapeutic, 30-40mmHg) is suitable for patients with severe varicose veins in the lower extremities with obvious edema or chronic lower extremity venous diseases with venous ulcers, as well as patients with lymphedema. The length of the stockings should be chosen based on the affected area.
Wear them during the day when you’re active, for at least 8 hours each day. Do not wear them when sleeping.
Moderate exercise is recommended after putting on the stockings.
Choose the right compression stockings. Choose the appropriate pressure based on leg symptoms, the length of the stockings based on the location of the varicose veins, and the appropriate size based on the dimensions of the leg, ankle circumference, calf circumference, and thigh circumference.
Even if only one leg has symptoms, it is still recommended to wear a pair.
Replace with new stockings every six months to a year.